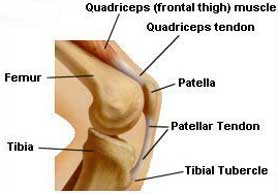
Patellar Tendinitis is an extremely common malady that can plague almost anyone, from athletes to laborers. It originally took on the nickname of "Jumper's Knee" because it frequently appeared in athletes who performed a lot of jumping and landing activity. Such exertions subject the knee to high shock-impact forces, which are one of the apparent causes of patellar tendinitis. The patellar tendon is a broad, thick, ligament-like structure that connects the lower portion of the patella (kneecap) to the prominent bump on the front of the upper tibia ("shin-bone") known as the tibial tubercle (see FIGURE 1). The patellar tendon is what doctors tap with a rubber hammer when they test your knee reflexes.
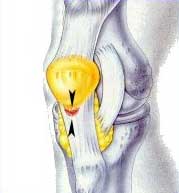
For unknown reasons, the insertion (attachment) of the middle fibers of the patellar tendon to the lower border of the patella is particularly vulnerable to mechanical irritation, inflammation and ultimately tendon fiber degeneration and breakdown (see FIGURE 2). The patellar attachment sites of the medial (inner side) tendon fibers and lateral (outer side) tendon fibers are much less commonly affected than that of the middle fibers. Under the microscope, the disease process associated with jumper's knee is characterized by cellular inflammation and degenerative breakdown of tendon fibers directly where the tendon attaches to the patella, and in more advanced cases, within the upper third of the tendon itself.
DiagnosisThe symptoms of patellar tendinitis are relatively easy to recognize. The patient will feel pain, not directly behind their kneecap (as in the condition of chondromalacia), but just below (distal to) it. Tenderness is present within the upper (proximal) patellar tendon, and in particular where its mid-section attaches to the lower end of the patella. The patient will typically feel discomfort there if they are either trying to kneel directly on their knee or if they are placing a lot of tension on their patellar tendon. The latter occurs while running, jumping or when bending the knee and supporting one's body weight at the same time (i.e., getting into a half-squat position). In very inflamed cases, local warmth can actually be felt emanating from the tissues beneath the skin overlying the patellar tendon. X-rays are almost always normal, and only in advanced cases where significant structural tendon degeneration has occurred are MRI scans (such as the one shown in FIGURE 3) abnormal.
Because most cases of patellar tendinitis are not advanced, and
therefore not diagnosable with an MRI scan, general physicians and even
orthopedic surgeons may sometimes fail to identify this common problem!
While the symptoms of jumper's knee are not hard to recognize if
one listens carefully to the patient's detailed description of what
they have been experiencing, specific diagnostic tests are often
required on physical examination to confirm the presence of this malady.
If the knee is examined for proximal patellar tendon tenderness at the
wrong joint flexion angle and/or with incorrect patellar posture, no
tenderness may be elicited and the diagnosis may therefore be missed.
During the course of rendering many second opinions over the years,
I have seen a number of cases where patellar tendinitis had been mistaken
for chondromalacia patella or knee arthritis, leading to an initial
recommendation for an unnecessary knee arthroscopy. TreatmentOnce diagnosed, and assuming that advanced tissue degeneration within the patellar tendon has not yet occurred, treatment is almost always initiated by non-operative means. A program of physical therapy may include quadriceps (frontal thigh muscle) stretching with special augmentation techniques, light conditioning exercise, multi-angle quadriceps isometrics, eccentric quadriceps strengthening, ice and friction massage to the tendon, dexamethasone iontophoresis, and sometimes ultrasound. Such therapy often proves effective, particularly when accompanied by oral anti-inflammatory medication. Obviously, avoiding the inciting stress or abnormal activity that caused the problem in the first place is helpful as well. Cases that prove unresponsive to activity modification, physical therapy and oral anti-inflammatory medication may often be successfully treated by way of appropriately administered corticosteroid (cortisone) injection. This treatment should be used very judiciously and only with proper injection technique, which usually involves placing a small dose of this anti-inflammatory medicine directly at the inflamed tendon-bone junction and an additional dose deep to (beneath) the upper tendon. In my experience, approximately 9 out of 10 cases of patellar tendinitis respond satisfactorily to non-operative treatment. However, if treatment is unsuccessful or if the condition is left untreated and allowed to progress, gradual tissue degeneration can weaken the patellar tendon and may occasionally result in spontaneous and unexpected tendon rupture during vigorous physical exertion. This is an unwelcome and sometimes catastrophic occurrence. In cases where advanced inflammatory degeneration has occurred within the upper tendon and/or in cases that have proven unresponsive to 6-12 months of non-operative management, surgical treatment is often the best option. A cure, or at least a significant improvement in symptoms, can usually be obtained by surgically excising the deteriorated tendon substance through a small skin incision located directly over the affected area. The small, unfilled space left by the excision of the chronically inflamed and degenerated tendon tissue gradually fills in with benign, fibrous scar tissue, usually bringing relief of the patient's pain. While the ability to kneel on hard surfaces in total comfort may never return, surgery often provides gratifying relief for many difficult cases of this condition.
|
||||||||||||||||||||||||